Heel Pain/Plantar Fasciitis
Our feet are under stress day in and day out, and when heel pain develops, it can make every step miserable. Fortunately, whether you're suffering from plantar fasciitis or another condition that causes heel pain, Foot and Ankle Center of Lake City's expert foot doctor, Dr. Rion Berg, can help you find relief. Learn more about the conditions we treat, as well as the wide range of treatment options we offer here.
Plantar Warts
Plantar warts can be ugly, embarrassing, and painful. This condition is common in children but can also occur in adults. Caused by the HPV or Human Papilloma Virus, plantar warts can spread to other parts of the body and to other people. At the Foot and Ankle Center of Lake City we offer the most advanced treatment for getting rid of plantar warts to get you back on your feet quickly.
 Fungal Toenails
Fungal Toenails
A fungal nail infection or onychomycosis can cause thick, discolored, brittle, and dystrophic toenails. In turn, this can make every step uncomfortable and make you too embarrassed to wear your favorite pair of open-toed shoes—and for diabetic patients, an untreated fungal infection can have particularly dire results. Don't let fungal nails endanger your health and self-esteem. Find out how Foot and Ankle Center of Lake City can help you find relief.
Ingrown Toenails
Ingrown toenails are a common condition that can make every step uncomfortable and, in some cases, lead to concerning infections. Don't let red, painful, swollen skin around an offending toenail force you to give up the activities you enjoy. At Foot and Ankle Center of Lake City, our talented and highly experienced podiatrist, Dr. Rion Berg, provides the gentle care and treatment you need to get back on your feet.
 Ball of Foot Pain
Ball of Foot Pain
Ball of foot pain can make every step you take excruciating. Fortunately, you don't have to let pain in the balls of your feet force you to stop doing the things you love. At Foot and Ankle Center of Lake City, our knowledgeable and highly-skilled podiatrist, Dr. Rion Berg, helps patients resolve their foot pain and regain their active lifestyles. Learn about common causes of ball of foot pain (such as Morton's neuroma, hallux rigidus, big toe joint pain, and metatarsalgia), their potential treatments, and how we can help restore your feet to health.
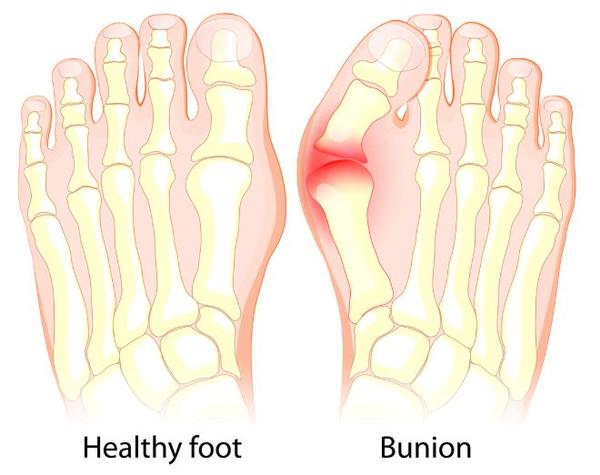 Bunions
Bunions
Bunions can be unsightly. But they can also making wearing shoes and walking very painful. At the Foot and Ankle Center of Lake City, podiatrist Dr. Rion Berg has successfully treated buion pain by using conservative to more advanced treatment. You don't need to put up with bunion pain. Find out more about how our clinic can provide relief.
 Hammertoe
Hammertoe
Hammertoe can disrupt your ability to play sports or find shoes you can wear pain free. Fortunately here at the Foot and Ankle Center of Lake City, podiatrist Dr. Rion Berg has the experience to help you manage hammertoe in it's early stages at home. For more advanced hammertoe, he has the surgical skills to eliminate your problem in the long term.
 Ankle Pain
Ankle Pain
Ankle pain can make weight-bearing, standing, walking, flexing your foot, and other movements difficult, causing you to miss out on the activities you enjoy. Fortunately, you don't have to let ankle pain stand in the way of your active lifestyle. Foot and Ankle Center of Lake City treats a wide range of podiatric conditions that cause ankle pain and offers conservative to advanced treatment options to meet your unique needs. Let our expert podiatrist, Dr. Rion Berg, and warm, friendly staff help you say "goodbye" to pain for good.
 Sports Injuries
Sports Injuries
Don't let a foot or ankle sports injury leave you sitting on the sidelines or missing out on the active lifestyle you enjoy. At Foot and Ankle Center of Lake City, our highly-experienced podiatrist, Dr. Rion Berg, provides expert treatment for a wide range of common podiatric sports injuries. Suffering from a sprained ankle, tendonitis, plantar fasciitis, or another sports-related injury to the feet or ankles? Find out how we can help you get back in the game as quickly and painlessly as possible.
 Pediatric/Children's Foot Problems
Pediatric/Children's Foot Problems
Habits for healthy feet are formed early. At the Seattle Center for Children's Foot Health at the Foot and Ankle Center of Lake City, we help children learn how to properly care for their feet, provide treatment for a range of common pediatric podiatry issues, and offer conservative to advanced options to meet your family's needs. Learn more about our podiatry practice and how to make an appointment with our expert podiatrist, Dr. Rion Berg, here.
 Hiking and Climbing Injuries
Hiking and Climbing Injuries
While hiking and climbing injuries are common there's a lot you can do to prevent them. In hikers, our office treats many patients with ball of foot pain and heel pain. Those who climb mountains or engage in rock climbing are highly prone to developing toenail problems. A key to preventing many of these problems is to ensure you have the right hiking shoes or boots for your particular sport and that they fit well. But as you'll learn below there are also other strategies you can use to keep you trekking.
Running Injuries
The Foot and Ankle Center of Lake City specializes in treating common foot conditions experienced by runners. Common running injuries we treat are plantar fasciitis, Achilles tendonitis, Morton's neuroma, bunions, and toenail problems such as fungus. Our office will evaluate your pain, treat it, and provide education to help you prevent it from coming back. Our goal is to ensure you can keep doing the sport you love.
 Skin and Toenail Conditions
Skin and Toenail Conditions
Many patients have skin and toenail conditions. While most of these conditions aren’t life-threatening, some can be painful, get worse over time, and spread to other people and other parts of the body. In this section, we describe these conditions and direct you to the right places on our website for more information.
